What Is Antibiotic Resistance and How Can You Help Prevent It?
Antibiotics have been one of the most important medical advancements in history. They’ve saved millions of lives by treating infections that were once deadly. But over time, some bacteria have evolved resistance to certain antibiotics. This global problem, known as antibiotic resistance, is one of the biggest threats to public health today.
What Is Antibiotic Resistance?
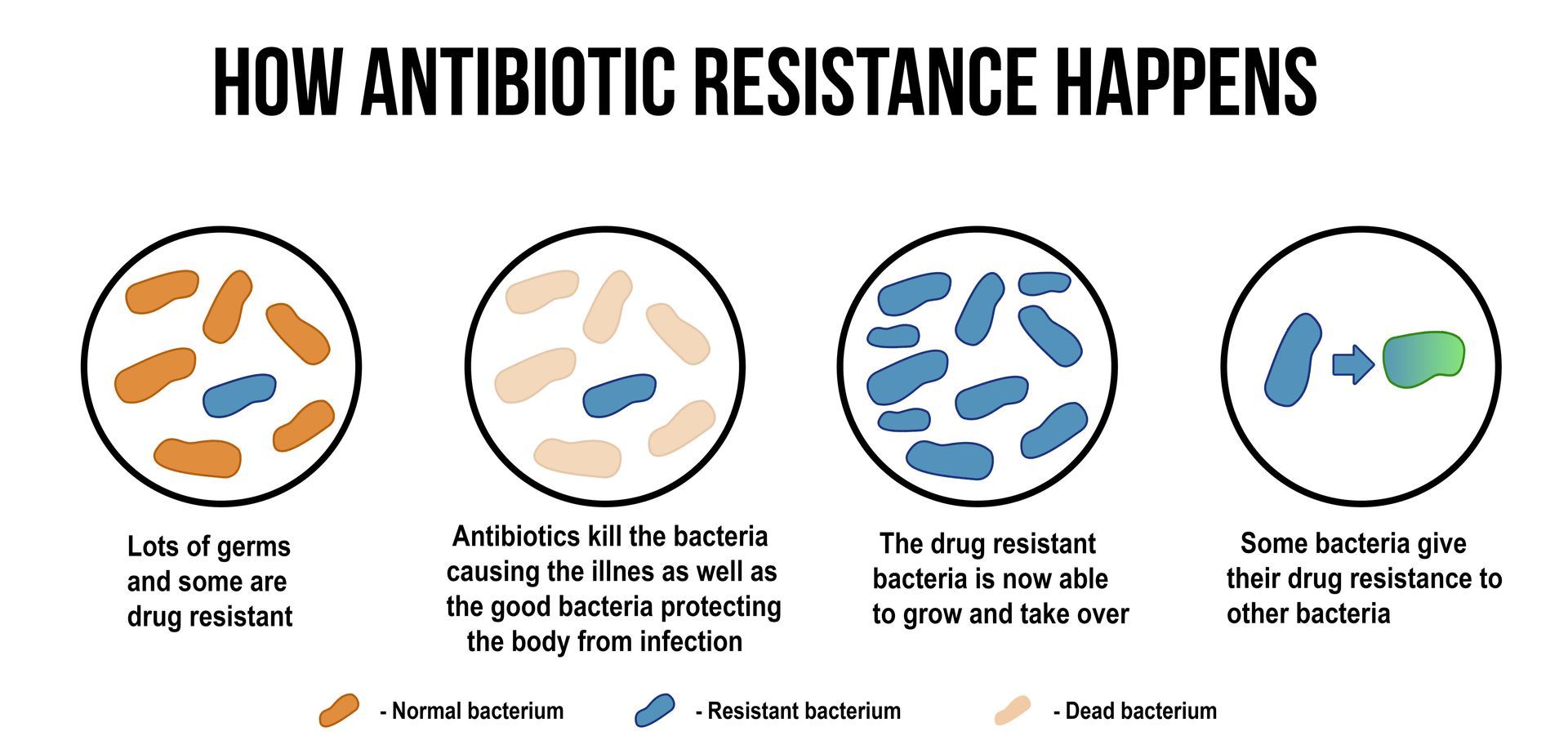
Antibiotic resistance happens when bacteria evolve in ways that make the drugs designed to kill them less effective. When antibiotics are used, they kill many bacteria, but some survive because of genetic mutations or natural selection. Those surviving bacteria then multiply, passing on their resistance traits. Over time, these resistant strains become stronger, harder to treat and can spread to others.
Why Antibiotic Resistance Is a Growing Concern
Antibiotic-resistant bacteria can turn common illnesses into serious health risks. Conditions like pneumonia, urinary tract infections and skin infections can become much harder to treat when standard antibiotics no longer work.
The Centers for Disease Control and Prevention (CDC) estimates that in the United States alone, more than 2.8 million antibiotic-resistant infections occur every year, resulting in at least 35,000 deaths annually. The problem is global, and it continues to worsen as resistant bacteria evolve faster than new antibiotics can be developed.
Antibiotic resistance also increases healthcare costs and lengthens recovery time. In severe cases, patients may need hospital care, intravenous medications or surgical procedures that could have been avoided if antibiotics had remained effective.
How Resistance Develops
Overuse of Antibiotics
Antibiotics are sometimes prescribed for illnesses caused by viruses, such as the flu or the common cold. Since antibiotics only work against bacteria, this type of misuse allows resistant bacteria to grow while providing no benefit to the patient.
- Incomplete Courses of Treatment
- Stopping an antibiotic too early can leave behind the strongest bacteria, which then multiply. Even if symptoms improve, it’s important to complete the full course of antibiotics exactly as prescribed.
- Use in Agriculture
- Antibiotics are often given to livestock to promote growth or prevent disease, even when animals are not sick. This can lead to resistant bacteria that spread through food, water and the environment.
- Global Travel and Transmission
- Resistant bacteria know no borders. People can carry them from one region to another, spreading infections quickly across communities and countries.
- Lack of New Antibiotics
- Developing new antibiotics is a long and expensive process, and fewer pharmaceutical companies are investing in it. This means resistant infections are growing faster than the availability of new treatments.
How You Can Help Prevent Antibiotic Resistance
Use Antibiotics Only When Necessary
Never pressure your healthcare provider for antibiotics if they are not needed. Colds, flu, bronchitis and most sore throats are caused by viruses, which antibiotics cannot treat. Trust your provider’s judgment about whether your illness requires antibiotic therapy.
Follow Directions Carefully
If your provider prescribes antibiotics, take them exactly as directed. Do not skip doses, share leftover medication or stop early because you feel better. Finishing the full course helps ensure all bacteria are destroyed and prevents survivors from developing resistance.
Avoid Self-Medicating
Never use leftover antibiotics or someone else’s prescription. Different infections require different medications, dosages, and durations. Taking the wrong antibiotic can delay proper treatment and increase the risk of resistance.
Stay Up to Date on Vaccinations
Vaccines help prevent infections that might otherwise require antibiotic treatment. Reducing the need for antibiotics also reduces the chances for resistant bacteria to develop.
Practice Good Hygiene
Simple habits such as washing your hands, cleaning surfaces, and preparing food safely help reduce the spread of infection. The fewer infections you get, the less you need antibiotics.
When Antibiotics Are the Right Choice
There are times when antibiotics are essential and lifesaving. Bacterial infections such as strep throat, bacterial pneumonia and urinary tract infections often require antibiotics to prevent complications. The key is to use them responsibly and under the guidance of a qualified healthcare provider.
If you’re unsure whether your symptoms are caused by a virus or bacteria, your provider can perform tests to determine the cause and prescribe the most effective treatment. Avoiding unnecessary antibiotic use protects your health and helps preserve these powerful medications for when they are truly needed.
Protect Your Health and Community in Bellaire, Conroe, Houston, Sugar Land and Dickinson.
Antibiotic resistance may sound like a global concern, but its prevention starts locally with responsible patients. Visit St. Hope Pharmacy or contact us here on our website to get your prescriptions filled and for trusted guidance on antibiotic use, safe medication disposal and personalized care.


